This is the first of five blogs on Healthcare Big Data and its impact written by John Morton about Big data for Digital Salutem. The second article is Big Data: Healthcare Prevention and the third Big Data: Healthcare Diagnosis
Medical data science and health informatics have been using big data methods and analytics, for longer than the term “big data” has been around. Admittedly they have been used in “back room” specialised departments hidden in the depths of medical research establishments.
However, today’s healthcare society faces the challenge of providing high-quality, patient-centred, sustainable and affordable healthcare, in an environment of increased demand and scarce resources. Here big data analytics, new computing technology and rethinking data relationships can drive new, exciting healthcare insights.
The last five years has seen a marked shift in the economics of computing capability, and birth of cost effective methods to digitalise information and a movement to democratise and share healthcare information (anonymised). Coupled with the ever increasing need to reduce the healthcare bill, greater emphasis is placed on using reliable technology to create better patient outcomes.
“Heath care spending will be the fastest growing item of government expenditure in the coming decades due to ageing societies, the expense of evolving technology, and widening coverage. In its analysis S&P said that by 2050 the costs would rise by 6 per cent of gross domestic product in the United Kingdom, Germany and France, as well as the United States and Japan. By mid-century health care costs will account for 11.1 per cent of GDP, up from 6.3 per cent in 2010.”
The use of existing and historical healthcare information, once allocated to dusty piles of paper based research is now digitalised and being made available. Globally health institutes, governments and health clinicians are providing more and more datasets of information for secondary uses. Allowing new ways to combine clinically vetted information.
Such initiatives allows institutes that may not have the resources, technical skills or capabilities to seek advice, help and support from those researchers individuals and institutes that are data hungry.
Healthcare is a very broad subject area and typically the research and the findings from healthcare reports focus on one aspect of healthcare (e.g. social enterprise companies that may focus on “Stroke”), or on delivery of healthcare (e.g. clinical, GP, Home care).
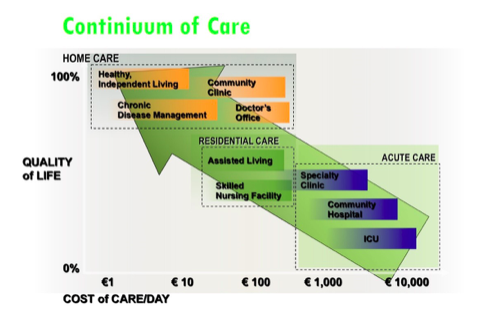
The promise of the “Internet of Things” and big data is not only to provide better continuous monitoring within these areas. It is to go far beyond this. It is to provide integrated end to end continuum of care (and wellness). In so doing, reduce the cost of overall healthcare provision.
Today’s technology for healthcare is both revolutionising healthcare and changing the deployment and manner of healthcare delivery. A smartphone today with the appropriate apps can confirm a number of things about YOU. You can test your eyesight and hearing, run Alzeheimer’s and dementia tests, connect to your Fitbit™ or Nike™ band (or many other products) and view fitness, exercise regimes, diet and hydration levels. Blood test analysers, vital monitoring and more are being added to these apps.
Healthcare delivery is also under threat. Previously, clinical staff were the keepers of medical knowledge and insight. Now with the internet and these new records of health fact, health practitioners now face the “educated health aware”. Their role is changing. This isn’t just about practitioners keeping “up to date“ with technology. This is about a wholesale education and learning challenge across healthcare. When a patient now speaks to a clinician they speak from an integrated set of symptoms, recorded information across their life, and some knowledge (not necessarily correctly deduced) from the internet.
All of this is a huge challenge for healthcare information custodians and guardians. Patient access to a patient’s medical records and the protection of patient information is expected, and deemed the norm. The health informatics professional has to reconsider and educate staff and the public on a range of topics about how health information can be used and when it shouldn’t be used.. The impact of this is redefining safety guidelines and safeguarding patients:
– Principles of Health Informatics
– Research Methods in Healthcare
– Information Systems in Healthcare
– Shared Care and Electronic Health Records
– Patient Safety and Clinical Risk
– Clinical Knowledge and Decision Making
– eHealth: Patients and the Internet
– Information Law and Governance in Clinical Practice
– Healthcare Quality and Evidence Based information Practice
– Using Information in Healthcare Management
– …. To name a few.
Over and above these specific areas, there is an additional external challenge. Other industries are now gathering and using “healthcare” information. This gathering and using information may be educating the public and setting a contrary value expectation to the public on the personal health information.
This is the first of five blogs on Healthcare Big Data and its impact. The remaining will consider big data for:
1. Big Data: Challenge, or Opportunity for Healthcare?
2. Big Data: Healthcare Prevention
3. Big Data: Healthcare Diagnosis
4. Big Data: Healthcare Treatment
5. Big Data: Healthcare Awareness
John Morton is a Big Data Advisor having with experience across the whole data value chain, business intelligence and analytics in a number of industries including clinical, healthcare informatics and Pharma. John’s has been fundamental in creating new medical IT solutions and medical devices for clinical environments; enabling the digital hospital; a physician on my shoulder; as well as the challenges and impact of technology within clinical environments.
More post: